Abstract
There are knowledge gaps regarding healthy lifestyle interventions (HLS) in fire academy settings and also regarding the impacts of the pandemic on training. We enrolled firefighter recruits from two fire academies (A and B) in New England in early 2019 as a historical control group, and recruits from academies in New England (B) and Florida (C), respectively, during the pandemic as intervention group. All three academies have similar training environments and curricula. Exposures of interest were a combination of (1) an HLS intervention and (2) pandemic impacts on curricula and training environments (i.e., social distancing, mask wearing, reduced class sizes, etc.). We examine health/fitness changes throughout training. The follow-up rate was 78%, leaving 92 recruits in the historical control group and 55 in the intervention group. Results show that an HLS intervention enhanced the effects of fire academy training on recruits’ healthy behaviors (MEDII lifestyle score, 0.5±1.4 vs −0.3±1.7), systolic blood pressure (−7.2±10.0 vs. 2.9±12.9 mmHg), and mental health (Beck Depression Score, −0.45±1.14 vs. −0.01±1.05) (all P < 0.05). The associations remained significant after multivariate adjustments. In addition, a 1-point increase in lifestyle MEDI during academic training is associated with about a 2% decrease in blood pressure over time, after multivariable adjustments (P < 0.05). However, the impacts of the pandemic restrictions on academy procedures compromised physical training, i.e. body fat percentage. l, push-ups and pull-ups.
Introduction
Accumulating evidence shows that firefighting can cause not only serious accidents and injuries1,2, but also chronic diseases3,4,5. Read also : Everything We Know About The New BTS Video Game ‘BTS Island: In the SEOM’. Occupational hazards such as chemicals, extreme temperatures, particulates, and high physical demands due to firefighting have been extensively researched,6,7 while emerging evidence reveals an unhealthy nutritional environment and sedentary behavior, which may contribute to lifestyle-related chronic diseases that are prevalent among firefighters3,8,9, including cancers, obesity, hypertension, cardiomegaly, coronary heart disease, and other cardiovascular diseases (CVDs)4,5,8,10.
Physical fitness is of great interest in the public safety workforce. Positive associations have been observed between physical fitness and training performance, lower rates of occupational injuries, lower risk of subsequent CVD events, and lower mortality11,12,13,14,15,16. Despite physical fitness requirements during academy training17, most fire departments do not require ongoing physical training and most firefighters are obese or overweight18. Studies have shown that fire academy training improves the health and fitness of fire recruits, but most of the benefits are lost soon after recruits become probationary firefighters17,19. A work environment that includes long periods of sedentary activity, inadequate fitness requirements, insufficient and interrupted sleep, and a culture that may encourage unhealthy diets contributes to obesity, poor physical fitness, and chronic disease risks9.
Several preventive strategies and interventions have been tried. The accumulation of exercise interventions and physical training programs carried out among firefighters show positive effects in improving body composition, aerobic capacity, muscle power, endurance and strength20,21. Other health promotion interventions, such as nutritional instruction and psychological resilience training, also have beneficial effects on professional firefighters’ body mass index (BMI), health behaviors, and mental health22,23,24.
Firefighter recruits are future firefighters who undergo academic training to be equipped with the professional skills and functional capabilities necessary for the fire service. In the US, fire academy training typically ranges from 12 to 20 weeks for career firefighters9. While existing evidence shows that academy training improves the physical fitness of firefighter recruits,17 our previous study showed that recruits’ blood pressure, both systolic and diastolic, increased by more than 2 mmHg on average during training , despite other improved health parameters19. Furthermore, in the same study, we found that traditional academic training did not improve the dietary behaviors of recruits19. To the best of our knowledge, while there have been quite a few intervention studies in career firefighters20,21,22,23,24, there is no behavioral health/lifestyle intervention research in firefighter recruits, although evidence has shown that early health education has a long time. -long-lasting health benefits25 and a healthy lifestyle (HLS) may be a potential solution to firefighters’ health problems9.
Since March 2020, the COVID-19 pandemic has affected millions of workers around the world26. While mitigation policies such as closures and remote work have been put in place, they are not applicable to essential occupations, including the training of new firefighters. Previous literature has demonstrated the risk of group transmission of SARS-CoV-2 infection (the virus that causes COVID-19) among fire academies and its associated impacts on mental health28. In fact, since fire academies needed to continue operating during the pandemic, some adjustments to the existing training curriculum were made to comply with public health regulations, such as the mandatory use of masks and increased social distancing. These adjustments include limiting class sizes, canceling large group activities, adjusting to social distancing during physical training, etc. Little is known about whether such adjustments influence the quality of academy training and its associated effects on the health and fitness of recruits. Therefore, we conducted this study to investigate the effects of (1) a healthy lifestyle intervention (HLS) and (2) an adjusted training curriculum due to the COVID-19 pandemic. , when comparing the recruits of the intervened academic classes with the historical controls.
Methods
Study design and study population
In this time-controlled intervention study, a historical control group was used to assess the effects of the interventions. This may interest you : Lessons Learned from Culturally Tailored Community Health. Therefore, two populations of firefighter recruits were enrolled; (a) the control group consisted of two classes of recruits undergoing academy training using existing pre-pandemic training curricula and (b) the intervention group consisted of two classes of recruits enrolled during the pandemic and also receiving an HLS intervention.
The control group was recruited in early 2019 from two fire academies (Academy A and B) in the New England area19,29. Both academies provide a 15- to 16-week training program that meets the standards of the National Fire Protection Association (NFPA), NFPA 1001: Standard for Professional Firefighter Qualifications. Except for minor differences between the two (for example, academy B requires recruits to spend the night at the academy on training days, while academy A recruits go home every day after training, and academy A academy B provides additional aquatics classes as part of their physical training), the recruits making up the historical control group at all academies were comparable based on our previous19 and current studies.
For the intervention group, we enrolled recruit firefighters from one fire academy in New England (academy B) and another in Florida (academy C) in late 2020. Training at academy C resembles that at academy B, regarding NFPA standards and the overnight requirement. , with similar training durations of 15 and 13 weeks for academies B and C, respectively.
All registered firefighter recruits who were over 18 years of age and gave informed consent were included. Those who did not consent to participate in the study or lacked essential demographic information (ie, age and gender) were excluded. The current study is part of the “Firefighter Recruit Health Study” approved by the Harvard T.H. Chan School of Public Health (IRB18-1902). We followed the Declaration of Helsinki throughout the study.
Selected health outcomes
Outcomes selected for the study included body composition, blood pressure, physical fitness tests, mental health assessments, and lifestyle behaviors. All academies except academy C had complete data collection, while academy C provided only subjective (ie, questionnaire) results. To see also : Lemley represented the United States at the Canada Cup. Related measurements were described in our previous studies19,29 and are summarized below.
The BMI and percentage of body fat of the recruits were examined as outcomes of body composition. A clinical stadiometer (portable stadiometer 213, SECA, Hamburg, Germany) and a bioelectrical impedance analysis (BIA) scale (BC-418 Segmental Body Composition, Tanita, Tokyo, Japan or InBody 230, Seoul, South Korea) in mode athletic trainers, operated by experienced fitness trainers or medical personnel, were used to retrieve the parameters. Measurements were taken at academy entry, midway through training (ie, week 8 for academy A and week 7 for academy B), and graduation from the academy. Body composition data was not available at Academy C.
Blood pressures were measured with an automated and calibrated sphygmomanometer (series 10, Omron, Kyoto, Japan), following professional guidelines30. Measurements were made before the recruits began their daily training or during rest. Each recruit was asked to rest in a seated position for at least 5 minutes before being measured in a seated position. The automatic sphygmomanometer would then take three readings, spaced 1 minute apart, and record an average. Blood pressure measurements were taken upon academy entry and graduation and were not available at academy C.
Selected fitness outcomes were push-ups, pull-ups, and 1.5-mile run time, with each measurement taken at academy entry, mid-training, and graduation. These are existing tests used by academies to assess the physical performance of recruits over time. Push-ups were determined as the number a recruit performed continuously in one minute, without breaking cadence. Pull-ups were counted as the number in a single trial with good cadence and overhand grip. The 1.5-mile run time was recorded in minutes. Physical fitness test results were not available at Academy C.
We used a questionnaire to examine participants’ mental health and lifestyle behaviors, which was administered upon entering the academy and upon graduation. The questionnaire consisted of components derived from validated questionnaires, incorporating a modified version of the Beck Depression Inventory for Primary Care (BDI-PC) (total score 0–18)31, Patient Health Questionnaire (PHQ-9) (total score 0–27). )32, and a modified version of the Post-Traumatic Stress Disorder Checklist (PCL-5) (total score from 0 to 76)33, where higher scores indicate poorer mental health. Regarding lifestyle behaviors, the questionnaire contained items necessary to calculate the MEDI-lifestyle score29, which is a 7-item healthy lifestyle score ranging from 0 to 7, including BMI, smoking history, dietary pattern (measured by the PREDIMED score, a 14-item Adherence Screener to the Mediterranean Diet34), physical activity35, sedentary behavior (measured by time spent watching television), daily sleep time, and afternoon naps. In particular, one point was awarded for each of the following: no smoking in the last 6 months, physical activity equivalent to more than 16 METs-h/week, PREDIMED score greater than or equal to nine points, BMI less than or equal to 30 kg/m2, television time less than 2 h/day, sleep time between 7 and 8 h/day and daytime nap; otherwise, each element would be given a value of 0.
Interventions
Compared to the historical control group, the intervention classes underwent the following changes to the existing training materials implemented by the academies.
First, the academies adopted an HLS intervention throughout the 13- or 15-week training based on the Mediterranean firefighter pyramid24, which illustrates a healthy lifestyle combination of balanced nutrition, regular physical activity, restful sleep, social connections, and positive family members with resilience strategies. , and the avoidance of tobacco and other toxic substances. Each participant received (a) access to a web-based toolkit (https://www.hsph.harvard.edu/firefighters-study/feeding-americas-bravest/) that includes information and resources for “Survival Mediterranean Style “, (b) a half-hour talk on a healthy lifestyle at the entrance to the training academy, (c) a sheet of waterproof plastic paper illustrating the Mediterranean pyramid of firefighters, (d) a magnet for the refrigerator with the Mediterranean pyramid on it, (e) weekly nutrition/lifestyle tips throughout the academy training, and (f) an introduction to meditation/breathing exercise apps (e.g., the Calm app (San Francisco, USA)). With the exception of (e), all intervention materials were delivered at the beginning of the training at the academy. Participants were able to review the HLS contents through the measures provided throughout the training period. While the practice of the HLS is voluntary, sponsored olive oil was supplied to the central kitchen at academy B and consumed by fire recruits when they stayed at the academy on weekdays, with academy C giving each recruit of the intervened class a WHOOP (Boston, USA) portable device that tracked the physical state and physiological parameters of the recruits. Notably, weekly homework, such as practicing a healthy recipe, was assigned along with weekly tips to recruits. with the co Working with the academies, extra training credits were awarded as an incentive if recruits showed adherence to the HLS outside of regular training hours.
Second, since the intervention classes were trained during the COVID-19 pandemic, some adjustments were made to the curriculum to align with public health policies. These changes included the use of required face masks at all times during training, limited class size, and switching from large group activities (such as group running) to small group fitness training to increase social distancing. Additionally, there was previously a weekly 1-hour aquatic training at the Academy B pool, but because the pool was closed, the aquatic classes were replaced with a weekly 1-hour joint mobility exercise, in which recruits performed a slow full body workout. stretching training at a pace similar to that of yoga.
Statistical analysis
Baseline characteristics and selected health outcomes were reported as mean ± standard deviation or median (Q1-Q3) for continuous variables after checking for normality, or number (%) for categorical variables, and compared between groups using t-test or Wilcoxon’s rank sum test, as appropriate, for continuous variables and Pearson’s Chi-square test with Yates’ continuity correction or Fisher’s exact test, as appropriate, for categorical variables.
In addition, we calculated changes in selected health outcomes over time during academy training by calculating the longitudinal difference “the measure at graduation, the measure at baseline” and presenting them as mean ± standard deviation. standard, after checking for normality. Differences in temporal changes between the intervention group and the control group were compared using t-test.
For multivariate adjustment, mixed-effects models incorporating the interaction term “Intervention Group × Time” were constructed to examine whether health changes over time during academy training differed between the two groups. Potential confounders based on our domain knowledge and baseline feature comparisons were included in the models. These are age, gender, starting body fat percentage, starting pushups, and/or starting BDI-PC scores.
Finally, we constructed multivariable fitted linear models to regress health changes on MEDI lifestyle score change, to demonstrate health changes per unit change in MEDI lifestyle score. For these models, changes in health throughout training were defined as percentage changes from baseline measurements, except for those variables with any value of zero at baseline (i.e., pull-ups, BDI-PC, PCL-5 and PHQ-9).
All reported P values are two-tailed and a P < 0.05 was considered statistically significant. We use R software (version 3.6.3) to perform the statistical analyses.
Sensitivity analysis
Regarding the differences in training between academies, we performed an additional sensitivity analysis that was limited to firing recruits at the academy with the available historical control class and intervention class, which is academy B. In fact , there was one more class at academy B that took place in early 2020, received the lifestyle intervention, but experienced an unexpected break in training for 3 months due to the initial outbreak of COVID-19. By comparing the three classes at Academy B (i.e., the historical control class, the COVID-19 interrupted class, and the intervention class), we were able to examine the effects of the intervention as well as the impact of training interruption. of 3 months in health of the recruits. Notably, only body composition and fitness testing data is available for the class interrupted by COVID-19.
In addition, although there were differences in intervention content between Academies B and C, as described above, we conducted secondary analyzes to investigate whether changes in health differed between the two populations (i.e., firefighter recruits who make up the intervention group of the academy). B and C, respectively) throughout the academy training. Since objective data were not available at Academy C, only subjective measures (ie behavioral and mental health outcomes) could be compared.
Ethics approval and consent to participate
The study is part of the “Firefighter Recruit Health Study,” which was approved by the Harvard T.H. Chan School of Public Health (IRB18-1902), and we followed the Declaration of Helsinki throughout the study.
Results
A total of 172 recruits were eligible for the main analyses, including 101 in the historical control group and 71 in the intervention group. Among them, 95 (94.1%) from the control group and 69 (97.2%) from the intervention group agreed to participate. After excluding those missing essential data (i.e., age and gender) and those who did not complete academy training, 92 (91.1%) in the control arm, comprised of 56 academy A and 36 from Academy B, and 55 (77.5%) in the intervention arm, made up of 37 from Academy B and 18 from Academy C, were included in the analyses.
There were no significant differences in the age of the recruits (28.6 ± 5.1 years vs 29.3 ± 5.2 years, P = 0.428) or gender (96.7% male vs 100.0% male). male, P = 0.293) between the two groups, while the control group showed a lower baseline body fat percentage (20.5±6.9% vs. 23.9±7.2%, P = 0.013) and performed more base push-ups (37.7 ± 14.1 vs. 28.7 ± 10.9, P < 0.001) than the intervention group. In addition, the intervention group reported more depressive symptoms (ie, higher BDI-PC score) at baseline (BDI-PC IQR: 0–1 vs. 0–0, P = 0.013) (Table 1).
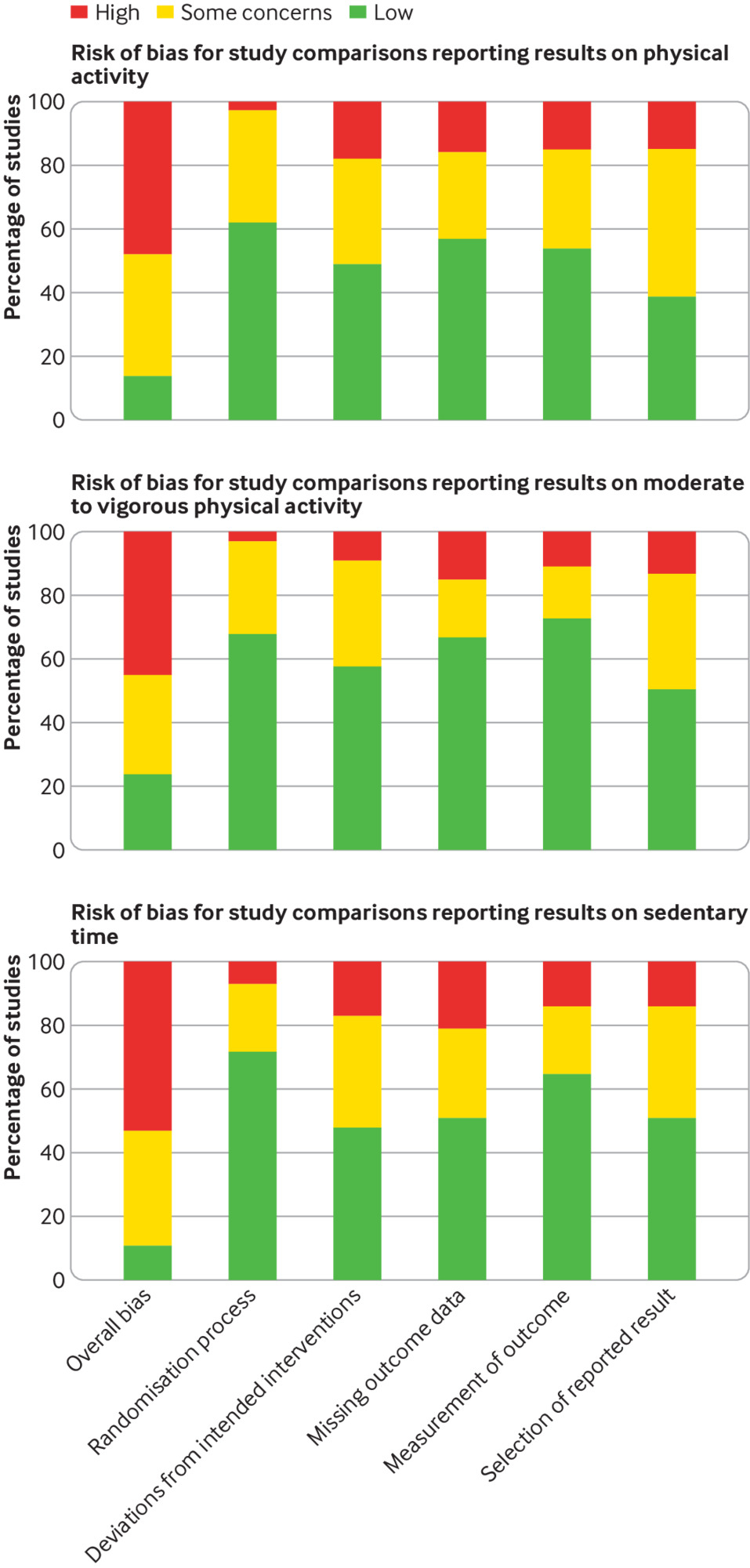
Table 2 demonstrates the changes in selected outcomes over time during academy training. Although both groups show a reduced percentage of body fat and an increase in push-ups and pull-ups throughout training, a smaller improvement is observed in the intervention group (percentage change in body fat: − 0.2 ± 2.8% vs − 1.8 ± 3.5%, P = 0.013; push-up change: 8.2 ± 4.9 vs 16.8 ± 10.4, P < < 0.001; pull-up change: 2.8 ± 2.5 vs 5.8 ± 0 = 0.1). On the other hand, the intervention group reported more improvements in lifestyle than the control group (change in MEDI-lifestyle score: 0.5 ± 1.4 vs −0.3 ± 1.7, P = 0.005) and a greater decrease in depressive symptoms ( change in BDI-PC score: −0.45 ± 1.14 vs −0.01 ± 1.05, P = 0.023). In addition, systolic blood pressure decreased in the intervention group but increased in the control group throughout academy training (−7.2 ± 10.0 mmHg vs. 2.9 ± 12.9 mmHg, P < 0.001) (Table 2, Fig. 1).
Box plots showing the distributions of selected recruits’ health profiles at baseline, mid-training, and upon graduation from the academy comparing (a) the historical control group (n = 92) and (b) the group intervention (n = 55). A. Body fat; B. systolic blood pressure; C. BDI-PC (Beck Depression Inventory for Primary Care); D. MEDI lifestyle score; E. push-ups; F. dominated. The plots were derived from recruits whose data were available at each time point. Post-hoc paired analysis with Holm’s adjustments was proved by *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. Body fat, systolic blood pressure, push-ups, pull-ups, and MEDI lifestyle score are only available for one academy in the intervention group (n = 37).
The associations remained significant after multivariate adjustments. Table 3 shows that the intervention group had fewer improvements in body fat percentage, push-ups, and pull-ups over time, but more improvements in the MEDI lifestyle score, systolic blood pressure, and the BDI-PC questionnaire. , after taking recruits into account. age, gender, baseline body fat percentage, baseline pushups, and/or baseline BDI-PC score (all P < 0.05 for the interaction term “Intervention Group × Time”).
To examine whether changes in health (i.e., the difference “measured at graduation, measured at baseline”) were related to changes in healthy lifestyle, we pooled both groups and constructed multivariable linear regression models. with the same covariates as the mixed models used for Table 3, with additional adjustments for different academic classes (ie, control group or intervention group) to account for intervention effects. Results show that a 1-point increase in lifestyle MEDI during academy training is associated with 1.95% and 2.73% decreases in systolic and diastolic blood pressure, respectively (both P < 0 .05). We found no significant associations between change in MEDI lifestyle score and selected other health outcomes (Table 4).
In sensitivity analyzes limited to academy B classes and adding one more class that received the healthy lifestyle intervention but suffered an unexpected 3-month training interruption due to the COVID-19 pandemic, we found no significant differences. on selected outcomes when comparing the intervention class to the control class. However, when comparing the COVID-19 interrupted class to the control, recruits’ BMI decreased 0.33 more per measurement time (i.e., baseline, mid-training, to graduation) than the control ( P = 0.036) after multivariable adjustments. However, the COVID-19 interrupted class shows an average of 1.3 fewer push-ups and 0.58 min of additional running time for a 1.5-mile run per measurement time than the control class (both P < 0.05 in multivariable adjusted mixed effects models). When comparing the COVID-19 interrupted class with the intervention class, the difference in 1.5-mile run time remained significant (0.58 min more per measurement time after multivariate adjustment, P < 0.001) (Supplementary Tables S1–S4, Supplementary Figure S1).
For secondary analyzes comparing health changes across academic training at academies B and C from the intervention group, there were no significant differences in changes in PREDIMED score, physical activity, sleep and napping behaviors, and the BDI-PC score. However, those from Academy C showed a greater decrease in TV viewing time (−1.21 ± 1.6 vs. −0.14 ± 1.7 h/d, P = 0.029), plus a decrease in the PCL-5 score (−4.3 ± 9.5 vs −0.2 ± 4.6 , P = 0.045), and a more decreased PHQ-9 score (−1.7 ± 3.0 vs. 0.0 ± 1.5) throughout the academy training.
Discussion
In our present intervention study with a historical control group, we investigated the combined effects of (1) a healthy lifestyle intervention and (2) an adjusted training curriculum due to the COVID-19 pandemic on health and the physical fitness of firefighter recruits during academy training. Our new findings show that the MEDI lifestyle score increased over time by 0.5 points more in the intervention group than in the control group, and self-reported systolic blood pressure and depressive symptoms had greater decreases during training. . In fact, each increase in the MEDI lifestyle score during the study period is associated with a 1.95% and 2.73% decrease in systolic and diastolic blood pressure, respectively. However, we also found that the intervention group had smaller reductions in body fat and improved less in push-ups/pull-ups than the control group, which is likely due to pandemic-required adjustments to the training curriculum. training.
To the best of our knowledge, the current work is the first lifestyle intervention study in a fire academy setting, although unfortunately it could not be a pure lifestyle intervention, but was affected by unprecedented adjustments. in the training curriculum due to the pandemic. It is biologically implausible to attribute the finding of higher MEDI lifestyle scores over time to pandemic-related restrictions on the curriculum. Therefore, lifestyle intervention is likely to improve recruits’ healthy lifestyle behaviors. In fact, a Swiss study investigating the effect of a healthy eating promotion program in career firefighters shows modest improvements in eating habits after one year of follow-up,36 although the findings were limited by the lack of a control group. and a small sample size (n = 28). Another study of fourteen volunteer firefighters showed that a 30-minute health promotion educational intervention increased participants’ health literacy37. Consequently, our results show that intervened firefighter recruits improved their HLS behaviors, using a well-defined control group, a more intensive lifestyle intervention, and an adequate follow-up period.
The significant decreases in blood pressure among the intervention group is another novel finding of our present study. For the control group, recruits who received the existing fire academy curriculum actually had increased blood pressure throughout training, despite better body composition and fitness. Given that hypertension and cardiovascular diseases are prevalent diseases in fire service personnel3,38, it is important to implement vascular health and blood pressure interventions39. In fact, evidence has shown that greater adherence to a healthy dietary pattern is associated with better cardiometabolic profiles40,41. Furthermore, our previous research on firefighter recruits also demonstrates a negative association between adherence to a healthy lifestyle and the prevalence of hypertension29. Consistent with the literature, we found that the healthy lifestyle intervention group had reduced blood pressure during academy training, and a one-point increase in the MEDI lifestyle score during training was associated with a decrease of about 2% in systolic and diastolic blood pressure, highlighting the efficacy of the healthy lifestyle intervention.
We found in the present study that recruits who attended academy training during the COVID-19 pandemic were more depressed at baseline. While the qualifying/entrance exams to become a firefighter remained the same, it’s not surprising that living through the pandemic was associated with an increase in recruits’ depressive symptoms at baseline. In fact, evidence has shown that psychological distress is a major public health problem among the general population in the midst of the pandemic42. Fear of being infected, feeling deprived of liberty due to quarantine and lockdown, social isolation, and concern about transmission between family members could contribute to substantial psychological impacts42,43,44,45,46. Fortunately, research shows that adopting a healthy lifestyle has benefits against depression. In an 8-year prospective study of 14,908 participants who initially did not have depression, optimal adherence to a healthy lifestyle (a combination of Mediterranean diet, increased physical activity, optimal sleep pattern, decreased sedentary period) was observed , no smoking, moderate alcohol consumption, optimal BMI , and positive social connections) was associated with a 32% lower risk of incident depression47. Consequently, we found that lifestyle-intervened recruits had more improved depressive symptoms during academy training than the historical control group. Furthermore, the findings of our secondary analyzes are indicative of the potential effectiveness of wearables on the mental and behavioral health of firefighter recruits, as those who received wearables (i.e., those in Academy C) reported more improvements. in TV viewing time, PCL-5 and PHQ-9 scores.
To our knowledge, there is no literature examining how pandemic-related adjustments in curricula might affect physical fitness. In our current study, the intervention group shows suboptimal training effects on recruits’ body fat and pull-up/push-up abilities, and a 3-month training cessation compromised the recruits’ aerobic fitness improvements (ie. , run 1.5 miles). In fact, research in the general population has shown that physical distancing and lockdown policies generally reduce people’s physical activity and fitness48,49. Despite the lack of evidence on firefighter recruits, firefighters, or other emergency responders, professional recommendations for training competitive athletes during the pandemic have been conservative, with less intensity and more flexibility50,51. Given that long-term detraining could decrease muscle mass, strength, and endurance,52 the decreased improvement in aerobic function observed among the interrupted class is not surprising. Additionally, a study of military recruits after a cluster outbreak of COVID-19 shows decreased fitness among affected personnel, compared to others receiving the same military training. Consequently, we found that a pandemic-adjusted academy training curriculum improved recruits’ fitness less than the historical control group. This is likely due to conservative changes made to training, reduced self-exercise during rest time, and possible subclinical/asymptomatic transmission among recruits. Therefore, future research is warranted to see if the effects and capabilities of academy training on physical fitness they will reach pre-pandemic levels as COVID-related restrictions relax and herd immunity rises (due to vaccination and prior infection).
The present study has several strengths. First, we adopted a time-controlled design, using a historical control group as a reference, which is the most rigorous study design in terms of research objectives. Although firefighter recruits receive academic training in groups, randomization at the individual level is inappropriate due to possible indirect effects54. Historical academy classes that had the same entrance qualification exams ensure interchangeability with intervention classes. In addition, we adjusted for potential confounders to estimate true associations. Third, almost all (> 94%) recruits in each group consented to participate in the study, and more than 75% of them completed the study follow-up. The relatively high rate of participation and follow-up minimizes potential selection bias. Finally, we use well-defined and validated tools to examine health outcomes, freeing the study from information bias.
However, there are some limitations in our study. One of them is that we cannot test the pure effects of a single intervention. In the current study, the differences in results are due to the combined effects of the two interventions (ie, a lifestyle intervention and training curriculum adjustments related to the pandemic). Although effects might differ based on existing literature and knowledge, there may be synergism or other interactions between the two interventions, preventing us from identifying pure effects due to either exposure. Second, objective measures for the intervention group are not available at Academy C, reducing the sample size and associated power for those outcomes. In addition, since the intervention classes were held in the midst of the pandemic, there may be unmeasured confounding factors related to the pandemic, such as decreased weekend physical activity and rest time, reduced of social contacts and less travel during the holidays. Finally, since the present study was designed to examine the combined effects of all HLS intervention measures, we were unable to say which individual measures are the most effective.
Conclusions
In conclusion, the present study shows that firefighter recruits who received a combination of a lifestyle intervention and COVID-19-related curriculum adjustments during academy training had more improvement than the control group. history with respect to HLS scores, blood pressure, and depressive symptoms. On the other hand, likely due to the pandemic’s impacts on training, the intervention group experienced less improvement in body fat, push-ups, and pull-ups. To examine actual changes due to the intervention, a future study enrolling additional post-pandemic academic classes that are more comparable to the historical control group and support a pure lifestyle intervention is warranted.
Data availability
The data sets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.
References
Orr, R., Simas, V., Canetti, E. & Schram, B. A Profile of Firefighter Injuries: A Critical Review. in t. J. Environment. Public Health Res. 16, 3931 (2019).
Article
Academic google
Frost, D.M., Beach, T.A., Crosby, I. & McGill, S. M. The cost and distribution of firefighter injuries in a large Canadian Fire Department. Work 55, 497–504 (2016).
CAS
Article
Academic google
Kales, S.N. & Smith, D. L. Fire suppression and the heart: Implications for prevention. Circulation 135, 1296–1299 (2017).
Article
Academic google
Soteriades, E.S., Kim, J., Christophi, C.A. & Kales, S. N. Cancer incidence and mortality in firefighters: a state-of-the-art review and meta-analysis. Asian Pac. J. Anterior Cancer. 20, 3221–3231 (2019).
Article
Academic google
Soteriades, E.S., Smith, D.L., Tsismenakis, A.J., Baur, D.M. & Kales, S. N. Cardiovascular disease in US firefighters: a systematic review. Cardiol. Rev. 19, 202–215 (2011).
Article
Academic google
Frost, D.M., Beach, T.A., Crosby, I. & McGill, S. M. Firefighter injuries are not just a fire scene problem. Work 52, 835–842 (2015).
CAS
Article
Academic google
Marsh, S. M., Gwilliam, M., Konda, S., Tiesman, H. M. & Fahy, R. Nonfatal injuries to firefighters treated in US emergency departments, 2003–2014. Am. Previous J. Medicine. 55, 353–360 (2018).
Korre, M., Smith, D. & Kales, S. N. Obesity and health in the North American Fire Service: Research points the way to positive cultural change. occupy medicine. (London). 68, 160–162 (2018).
Article
Academic google
Sotos-Prieto, M., Jin, Q., Rainey, D., Coyle, M. & Kales, S. N. Barriers and solutions to improve nutrition among fire academy recruits: a qualitative evaluation. in t. J. food science. Nutrition 70, 771–779 (2019).
Article
Academic google
Kales, S.N., Soteriades, E.S., Christophi, C.A. & Christiani, D. C. Emergency duties and deaths from heart disease among firefighters in the United States. N. English J.Med. 356, 1207–1215 (2007).
CAS
Article
Academic google
Bakker, E.A., Sui, X., Brellenthin, A.G. & Lee, D.C. Physical activity and fitness for the prevention of hypertension. Current Opinion Cardiol. 33, 394–401 (2018).
Article
Academic google
Baur, D.M., Christophi, C.A., Tsismenakis, A.J., Cook, E.F. & Kales, S. N. Cardiorespiratory fitness predicts cardiovascular risk profiles in career firefighters. J. Occupy. Reign. Medicine. 53, 1155–1160 (2011).
Article
Academic google
Bycura, D.K., Dmitrieva, N.O., Santos, A.C., Waugh, K.L. & Ritchey, K. M. Efficacy of a goal setting and implementation planning intervention on cardiorespiratory fitness of firefighters. J. Force Cond. Res. 33, 3151–3161 (2019).
Article
Academic google
Yang, J. et al. Association between push-up exercise capacity and future cardiovascular events among active adult men. JAMA Network Open. 2, e188341. https://doi.org/10.1001/jamanetworkopen.2018.8341 (2019).
Korre, M. et al. Recruit fitness and police academy performance: a prospective validation study. occupy medicine. (London). 69, 541–548 (2019).
CAS
PubMed
PubMed Center
Academic google
Durand, G. et al. Physical activity of firefighters: Relationship with physical fitness and risk of cardiovascular diseases. Medicine. science Sport exercise. 43, 1752–1759 (2011).
Article
Academic google
Cornell, D.J., Gnacinski, S.L., Meyer, B.B. & Ebersole, K. T. Changes in health and fitness in firefighter recruits: an observational cohort study. Medicine. Sports science. Exercise 49, 2223–2233 (2017).
Article
Academic google
Poston, W.S. et al. The prevalence of overweight, obesity, and poor physical fitness in a population-based cohort of firefighters. J. Occupy. Reign. Medicine. 53, 266–273 (2011).
Article
Academic google
Lan, F.Y. et al. The effects of fire academy training and probationary firefighter status on selected basic measures of health and fitness. Medicine. science Sport exercise. 53, 740–748 (2021).
Article
Academic google
Andrews, K.L., Gallagher, S. & Herring, M. P. The effects of exercise interventions on the health and fitness of firefighters: a meta-analysis. Scan. J.Med. Sports science. 29, 780–790 (2019).
Article
Academic google
Hollerbach, B.S., Jahnke, S.A., Poston, W.S.C., Harms, C.A. & Heinrich, K. M. Examination of a novel exercise training program for firefighters on simulated fire ground test performance, cardiorespiratory endurance, and strength: a pilot investigation. J. Occupy. Medicine. Toxicol. 14, 12 (2019).
Article
Academic google
Antonio, J. et al. Interventions for the prevention and management of occupational stress injuries in first responders: a quick overview of reviews. system Rev 9, 121 (2020).
Article
Academic google
MacMillan, F., Kolt, G.S., Le, A. & George, E. S. Systematic review of randomized controlled trial health promotion intervention studies in fire services: study characteristics, intervention design, and health impacts. occupy Reign Medicine. https://doi.org/10.1136/oemed-2020-106613 (2020).
Korre, M., Sotos-Prieto, M. & Kales, S. N. Survival Mediterranean Style: Lifestyle Changes to Improve Health for the US Fire Service Front. Public health. 5, 331 (2017).
Article
Academic google
Messineo, A., Cattaruzza, M.S., Prestigiacomo, C., Giordano, F. & Marsella, L. T. Sustainability of prevention practices at work: Safety, simplification, productivity and efficiency. Ana. I G. 29, 407–421 (2017).
CAS
Acknowledgements
PubMed
Funding
Author information
Authors and Affiliations
Academic google
Lan, F.-Y., Wei, C.-F., Hsu, Y.-T., Christiani, D. C. & Kales, S. N. Work-related transmission of COVID-19 in six Asian countries/areas: a follow-up study. Plus one. 15, e0233588. https://doi.org/10.1371/journal.pone.0233588 (2020).
Lancet, T. The plight of essential workers during the COVID-19 pandemic. Lancet 395, 1587 (2020).
Article
Academic google
Walecka, I. et al. Psychological consequences of hospital isolation during the COVID-19 pandemic: research on the sample of Polish firefighting academy students. current psychology https://doi.org/10.1007/s12144-021-01982-3 (2021).
Lan, F.-Y. et al. A Mediterranean lifestyle is associated with a lower prevalence of hypertension and better aerobic capacity among New England firefighter recruits. J. Occupy. Reign. Medicine. 62, 466–471 (2020).
Article
Academic google
Whelton, P.K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guidelines for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Group Cardiology/American Heart Association Working Group on Clinical Practice Guidelines. Hypertension 71, 1269–1324 (2018).
Contributions
CAS
Corresponding author
Article
Ethics declarations
Competing interests
Additional information
Publisher’s note
Academic google
Supplementary Information
Rights and permissions
Winter, L.B., Steer, R.A., Jones-Hicks, L. & Beck, A. T. Screening for major depressive disorders in adolescent medical outpatients with the Beck Depression Inventory for primary care. J. Teenagers. Health. 24, 389–394 (1999).
About this article
Cite this article
CAS
Article
Comments
Can COVID-19 spread through HVAC systems?
Academic google
Spitzer, R.L., Kroenke, K. & Williams, J. B. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Evaluation in Primary Care of Mental Disorders. Patient Health Questionnaire. JAMA. 282, 1737-1744 (1999).
How long can the coronavirus stay in the air?
Ashbaugh, A.R., Houle-Johnson, S., Herbert, C., El-Hage, W. & Brunet, A. Psychometric validation of the English and French versions of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5). Plus one. 11, e0161645. https://doi.org/10.1371/journal.pone.0161645 (2016).
How can I improve ventilation at home to prevent COVID-19?
Papadaki, A. et al. Validation of the English version of the 14-item Mediterranean diet adherence questionnaire of the PREDIMED study, in people with high cardiovascular risk in the United Kingdom. Nutrients 10, 138 (2018).
What is the risk of contracting COVID-19 while exercising?
Article
Why the air at the gym may be more likely to spread COVID-19?
Academic google
Can I excercise outdoors during the coronavirus pandemic?
Godin, G., Jobin, J. & Bouillon, J. Assessment of leisure-time exercise behavior by self-report: a concurrent validity study. They can. J. Public Health. 77, 359–362 (1986).
What are the common side effects of COVID-19 vaccines?
CAS
PubMed
When do COVID-19 vaccine side effects appear?
What are the common side effects of the COVID-19 vaccine?
Academic google
Is it good to buy frozen fruits and vegetables to eat during the COVID-19 pandemic?
Bucher Della Torre, S., Wild, P., Dorribo, V., Amati, F. & Danuser, B. Eating habits of professional firefighters: Comparison with national guidelines and the impact of the healthy eating promotion program. J Occupy Environment. 61, e183-e90 (2019).
Palms. & Yoos, J. L. Health promotion in volunteer firefighters: evaluation of knowledge of the risk of developing cardiovascular diseases. Health safety in the workplace. 67, 579–583 (2019).
How should I wash fruits and Vegetables after bringing them from super market during COVID-19 pandemic?
Article
Can I get the coronavirus from food, food packaging, or food containers and preparation area?